- Special Issues-06-01-2016
- Volume 31
- Issue 6
Raman Spectroscopy as a Tool for Analytical Quality Control in a Hospital Environment
Analytical quality control (AQC) is an established application of Raman spectroscopy in many industrial fields. The extension of Raman spectroscopy as an AQC method in hospital environments imparts the benefits of a noninvasive and nondestructive analysis. The literature in using Raman spectroscopy as an AQC method for chemotherapy preparation and anesthesia gas monitoring is reviewed. Future applications in tissue engineering and incorporating new Raman techniques into AQC are also discussed.
Analytical quality control (AQC) is an established industrial application of Raman spectroscopy. The extension of Raman spectroscopy as an AQC method in hospital environments imparts the benefits of a noninvasive and nondestructive analysis. The literature related to using Raman spectroscopy as an AQC method for chemotherapy preparation and anesthesia gas monitoring is reviewed. Future applications in tissue engineering and incorporating new Raman techniques into AQC are also discussed.
Raman spectroscopy is an optical spectroscopy technique that is commonly used for materials analysis. The “molecular fingerprint” provided by Raman spectroscopy enables chemical analysis in polymer, chemical, and pharmaceutical industries. The specificity and sampling versatility of Raman spectroscopy are attractive features for biomedical applications, especially for disease diagnostic purposes. There are myriad literature reports of in vivo Raman spectroscopy for biofluid, tissue, or cell analysis (1â3). Diagnostic applications range from bedside or at-patient measurements, integration into a clinical chemistry laboratory, to high-throughput tissue section analysis in a pathology core facility. From the many literature reports, there is a clear trend of moving Raman spectroscopy into a hospital environment.
There is scant number of reports describing the use of Raman spectroscopy in a hospital environment that were not related to disease diagnosis. To satisfy a curiosity, I sought out literature reports of Raman spectroscopy applications in a hospital environment. Two major applications were found in the literature: analytical quality control (AQC) for compounded formulations and gas analysis during general anesthesia. In this article, I review the literature for these two applications. I also highlight exciting technologies that may accelerate the development of potential applications.
Methods
The ISI Web of Science database was used to identify 62 articles containing the terms ‘‘Raman spectroscopy’’ and ‘‘hospital.’’ Articles describing Raman spectroscopy of tissue, biofluids, and cells for possibly diagnosing disease were excluded. The initial search resulted in six articles, all regarding the use of Raman in AQC. References of the initial six articles were then searched for additional articles. U.S. patents were searched, but were excluded from the review. One patent review resulted in the discovery of patent US4648714A “Molecular Gas Analysis by Raman Scattering in Intracavity Laser Configuration,” which describes Raman spectroscopy for anesthesia gas analysis. This finding piqued my curiosity, and I performed a literature search on the patent authors in ISI Web of Science. That search revealed the history of a commercial Raman spectrograph for anesthesia gas analysis.
Applications
AQC for Compounded Formulations
AQC is an established application of Raman spectroscopy in the pharmaceutical field (4,5). Most pharmaceutical products are prepared by the manufacturer in a consumable form such as a solid dose or drinkable liquid form. Some pharmaceutical products, such as chemotherapies, anti-inflammatories, anti-infectives, or monoclonal antibodies, require the final product to be prepared at the hospital pharmacy in a process known as compounding. For these compounded formulations, also called therapeutic objects (TO) in the literature, an active pharmaceutical ingredient (API) is diluted with dextrose, saline, or water and then is added to a prelabeled package. The package can be a syringe, a single-use infusion pump, or an infusion bag.
Safely delivering the correct dose to the patient is an ethical obligation. In France, it is also a legal matter and France requires strict control of chemotherapy or cytotoxic preparations (6,7). The safety and health of health-care professionals who handle these medicines is another serious concern. Typically, these medicines are cytotoxic, radioactive, or carcinogenic and chronic or accidental exposure represents a serious health risk for health-care professionals. According to the U.S. Centers for Disease Control (CDC), 8 million health-care professionals are potentially exposed to hazardous medicines (8). Early research showed exposure-related health issues in pharmacists, nurses, and other health-care staff who prepared, administered, or disposed of hazardous medicines (9). As a result of those studies, the CDC has issued updated guidance on how to reduce exposure risk by using appropriate personal protection equipment, biosafety cabinets, equipment handling, and waste handling. Even so, there are continued reports of improper vial cleaning or incomplete staff training that may represent a continued risk of accidental exposure (10,11). Any analyzed product must also be disposed of under strict regulations since the formulations are an environmental waste hazard. The variety of molecular properties and delivery systems, combined with safety and environmental concerns, has underscored the need for a rapid, noninvasive, and specific analytical method for therapeutic objects.
Analytical methods used to quantify chemotherapies were assessed by Bazin and colleagues (7) for their performance, safety, and logistical attributes. High performance liquid chromatography (HPLC) or flow-injection analysis (FIA) methods are the most commonly used methods because of their specificity, low-cost, reliability, accuracy, and low limits of quantification. However, there are drawbacks to HPLC or FIA including sample extraction and preparation and incompatibility with low-volume delivery systems. Raman spectroscopy has been proposed as a complementary technique because it provides noninvasive and nondestructive analysis. A comparison of Raman-based AQC with HPLC demonstrates the feasibility of Raman in the therapeutic range for many compounds and delivery systems.
Raman spectroscopy for AQC of pharmaceutical preparations was first reported in 2006 (12). Fourier transform (FT) Raman was used to quantify diclofenac or aminophylline in injection solutions. FT-Raman predictions of API concentrations were compared to ultravioletâvisible (UVâvis) reference measurements. Aqueous solutions of diclofenac or aminophylline were prepared with standard excipients and methods, with varying amounts of API. Acetonitrile was used as an internal standard to standardize spectral intensity, and API and excipient concentrations were shown to be independently varying in the studied solutions. Quantification of the API was demonstrated through univariate (band integration) and multivariate (partial least squares [PLS] and principal components regression [PCR]) analysis or unnormalized and intensity-normalized spectra. PLS resulted in a more robust model, with the lowest relative standard error of prediction and the highest correlation with reference measurements (R2 > 0.99 for diclofenac and aminophylline). The model was then applied to FT-Raman analysis of five commercial preparations containing 25 mg/mL of the API. API concentration, predicted by Raman, was 21.3 ± 0.8 mg/mL of aminophylline and 24.7â25.7 mg/mL for diclofenac. It was noted that despite the low Raman signal, Raman-calculated API concentrations were close to concentrations obtained using the reference UVâvis method.
A research group in the Clinical Pharmacy department at the Necker-Enfants Malades hospital in France has made important contributions in developing Raman for AQC of compounded formulations. In their first reported study in 2012 (article in French), Bourget and colleagues (13) demonstrated that a Raman method provided good repeatability, reproducibility, and accuracy in quantifying two anthracycline medicines: adriamycin and epirubicin. Correlation tests showed that Raman was noninferior to HPLC, and may be a rapid and noninvasive alternative AQC method for these medicines (13). Three reports from the group extended the applicability of Raman to other molecule classes, including fluorouracil, ganciclovir, and camptothecin analogs, and to other delivery systems including portable infusion pumps (14,15).
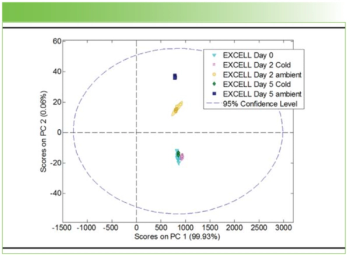
Portable infusion pumps are single-use, single-flow devices for delivering medicines in a home setting, delivering for 12 h to 7 days. Portable infusion pumps are convenient delivery systems and enable the patient to receive a prolonged dose without needing to be in a hospital. But the formulation must first be prepared at the hospital or care facility’s pharmacy, with the associated quality controls. Simultaneous measurement of the API, solubilizing matrix, and infusion pump was demonstrated by Bourget and colleagues in 2014 (16). A widely used chemotherapy, 5-fluorouracil, was compounded into an elastomeric portable infusion pump. A 785-nm Raman spectrograph, equipped with a noncontact optic, collected Raman signal for 1 min. Raman spectra of the API and dextrose or saline matrix were taken directly through the polymeric pump. HPLC of the Raman-examined formulations provided reference measurements. Spearman and Kendall correlation tests were used to test the hypothesis that Raman and HPLC values are “strictly identical.” Spearman (r > 0.93) and Kendall (t > 0.93) correlation tests showed that Raman-calculated API concentrations were highly correlated with HPLC values. Although the HPLC measurements had higher precision and accuracy, Raman spectroscopy provided suitable quantification, accuracy, and linearity in the concentration ranges encountered clinically.
The performance of a compact and benchtop Raman spectrometer were compared in an AQC study of two chemotherapy agents: irinotecan and toptecan (6). Raman-derived concentrations using the benchtop spectrograph, with 350-mW laser power at 780 nm, were shown to be highly correlated with reference HPLC measurements for both therapeutic agents. Raman-derived concentrations using the compact system, with 150-mW laser power at 780 nm, provided acceptable quantification of irinotecan but not toptecan. The authors point out that the clinical dose of toptecan is 32â56-fold lower than irinotecan, which may account for the inability of the compact Raman spectrometer to quantify the low-dose formulations.
A comprehensive 18 month longitudinal study using a combined UVâRaman analyzer on 5742 preparations was reported by Nardella and colleagues (17). In this study, UVâvis was used to quantify API while Raman was used to examine the solvent of dextrose or saline. Volume correction of solvent bags was achieved using a weighing method. Qualitative analysis of the formulations was effective, and more than 99% of APIs and solvents were identified. The authors used the results of the 18-month study period to identify recurrent nonconforming formulations and improve their production. For low-dose formulations, preparation and analyzer limit of detection were found to be critical in API quantification.
Budget, safety, operator training, method development, disposables, and instrument maintenance are important considerations in choosing an analytical method. With respect to analytical methods in AQC for compounded formulations, two studies showed that there is no overtly superior technique (7,18). In those papers, Raman was shown to be cost effective, rapid, broadly applicable, compatible with a variety of delivery devices, and reduced the risk of exposure for hospital staff. The noninvasive nature of Raman also eliminated the need for consumables and alleviated environmental concerns regarding disposing hazardous waste. HPLC was considered to be the gold standard technique because of its superior quantification and broad implementation.
Approximately 90% of compounded formulations are delivered by infusion bag. Bazin and colleagues were rightly skeptical about Raman’s capability for measuring low doses through the infusion bag, especially since there are no literature reports of directly measuring in an infusion bag. Yet currently available technology may be able to address this important concern. Spatially offset Raman spectroscopy (SORS) is routinely used for noninvasive and direct analysis of forensic or pharmaceutical samples through plastic containers. A recent study by Buckley and colleagues (19) demonstrated the feasibility of micro-SORS to measure red blood cells through sealed plastic blood storage bags, and these principles can be applied to measurements in infusion bags. I look forward to the incorporation of spatially offset or transmission Raman techniques to examining compounded formulations directly in infusion bags.
Gas Monitoring During General Anesthesia
Anesthesia is an important aspect of an operation, providing pain relief and enabling a safe surgical procedure. A patient may be locally, partially, or generally anesthetized, depending on the surgery. Local anesthesia provides pain relief to a small part of the body, such as a tooth or joint injection site, and includes topical or site-specific injection. The patient is typically awake during surgeries requiring local anesthesia. Partial anesthesia can be applied to a larger region of the body, such as an arm or spine, and includes an epidural or spinal block. Depending on the patient, a medication may be added to help the patient sleep or relax during surgeries requiring partial anesthesia. General anesthesia provides full-body pain relief, and includes injected or inhaled medicines. The patient is fully asleep during surgeries requiring general anesthesia, and their respiration, blood pressure, and body temperature are monitored.
Monitoring respired and anesthetic gases during general anesthesia are important to ensuring patient safety. Monitoring exhaled carbon dioxide (CO2), also called end-tidal carbon dioxide (EtCO2), ensures proper ventilation. EtCO2 monitoring is mandatory for patients using an endotracheal or laryngeal mask airway for general anesthesia, and is especially important in monitoring patients who are at high risk for retaining CO2 (20). The term capnography encompasses analytical methods used to measure and display a visual waveform recording of exhaled CO2 (21).
In addition to capnography, gas flow, oxygen, and volatile anesthetic agents such as halothane, enflurane, and isoflurane are monitored and quantified (22). Infrared (IR) spectroscopy is typically used in capnography, even though mass spectrometry (MS) is more accurate. Starting in the late 1980s, Raman spectroscopy was used to measure respired and anesthesia gases. The specificity, versatility, and capability of monitoring several gases simultaneously were attractive features of Raman spectroscopy that lead to its commercial development as an anesthesia gas monitor called the Rascal I (1986â1993) and later the Ohmeda Rascal II (1994â1998).
In the first report of Raman spectroscopy of respired and anesthesia gases, Van Wagenen and colleagues (23) demonstrated feasibility using a research-grade benchtop Raman spectrograph and a custom-built portable Raman gas analyzer operating at 488 nm. Reference gases and mixtures were examined by a benchtop Raman spectrometer, a custom-built prototype clinical Raman instrument, and an IR gas analyzer. These studies demonstrated a rapid 67-ms response of the prototype analyzer at a clinically relevant flow rate of 150 mL/min. Sharp bands allowed measurement of oxygen, carbon dioxide, nitrogen, nitrous oxide, and the volatile agents halothane, enflurane, and isoflurane. Some signal overlap was observed in the anesthetic gases and in nitrogen and nitrous oxide, which was accounted for by linear matrix analysis. Raman gas analyzer measurements were highly correlated with reference measurements (R2 > 0.99).
The feasibility of in vivo gas monitoring by Raman spectroscopy was demonstrated in a pilot study of 10 patients (24,25). The Rascal I Raman gas analyzer weighed 70 lb, required a cooling fan and drew 8 A at 110 V. Importantly, no adverse effects were observed throughout the study. Continuous measurements allowed examination of oxygen, carbon dioxide, nitrogen, nitrous oxide, and volatile anesthetic gases every 10 min. Reference MS measurements were collected simultaneously with the Raman measurements, but breath-to-breath direct comparisons could not be made because of slight sampling differences. In this pilot study, Raman was shown to provide waveforms similar to MS and was compatible with operating room workflows. Compatibility of the Rascal gas analyzer with magnetic resonance imaging (MRI) was demonstrated in pediatric patients requiring anesthesia to undergo an MRI (26). In an extraordinarily comprehensive study of instrument performance, Lawson and colleagues (27) examined 21 Rascal gas analyzers where they assessed instrument long-term stability and reliability for 29 months. Signal linearity was acceptable for oxygen, nitrogen, carbon dioxide, and nitrous oxide, even though the instruments had not undergone a calibration in more than two months. However, regular calibrations were recommended to avoid drift in volatile anesthetic agent signals and even calibrated instruments routinely overestimated the concentrations of volatile agents.
The Rascal II was a combined Raman gas analyzer and pulse oximeter introduced by Ohmeda in 1994. A description and image of the Ohmeda Rascal II is available from the Wood Library-Museum (28). The on-line drawing belies the instrument heft, as it weighed 23 kg (51 lb), and its large dimensions of 246 x 356 x 526 mm (~9.7 x 14 x 20.7 in.) (29). Despite its size, heft, and “finicky” behavior, the Rascal II analyzer filled an important gap in analyzing anesthesia gases including end-tidal nitrogen for bubble detection and low-flow anesthesia because the analyzed gas sample could be returned to the breathing system (29). Raman spectroscopy is well-regarded in the anesthesiology community (30,31) and an essay in the Bulletin of Anesthesia History highlights the legacy of C.V. Raman and the history of “the Little Rascal” (30).
Since the discontinuation of the Rascal II in 1998, there have been many advances in laser, detection, and software technologies. I was delighted to see a renewed interest in this application, which focuses on Raman spectroscopy of anesthesia gases at low pressure (32,33). Two sample chambers were developed and compared using calibration gases. A near-confocal sample chamber showed better performance than a highly reflecting sample chamber that enabled multiple scattering. Calibration gas mixtures were tested in the laboratory and in a human patient simulator, which mimics human breathing behavior. Raman measurements of oxygen, nitrogen, carbon dioxide, water, and volatile agents were compared to a clinical anesthesia gas monitor. These promising preclinical experiments demonstrated the feasibility of their approach in simultaneously quantifying anesthesia and respiration gases.
Future Prospects
Technological advances in nanofabrication, automated assembly and user interfaces have enabled miniaturized and handheld Raman instruments for use by nonspecialists. Raw materials identification in forensic and security applications are the primary use for handheld or portable systems, and the measurement principles could be applied in a hospital setting. SORS, transmission Raman, and surface-enhanced Raman are exciting technological developments that can also expand hospital-based applications for Raman spectroscopy. The extension of Raman spectroscopy to tissue or cell quality control has been explored in academic laboratories for quality control for sterilized cartilage tissues for grafts or tissue engineering (34,35), and bone tissue (36â38).
Conclusions
Raman spectroscopy has a valuable place in hospital environments for analytical quality control. Real-time, nondestructive analysis provided by Raman is well-suited for compounded formulations or anesthesia gas analysis. While the literature reports mainly come from academic groups, the groups are associated with a hospital and the projects have active clinical collaborators. It is also possible that hospitals have developed Raman spectroscopy applications in-house that are not reported in the literature. I look forward to new hospital, life science, and tissue engineering research that incorporates Raman spectroscopy into its suite of analytical tools.
Acknowledgments
I thank Ian Lewis and Lisa Ganster at Kaiser Optical Systems Inc., and Blake Roessler and Michael Morris at the University of Michigan for their support. I also thank Francis Esmonde-White for editorial comments.
References
- L.-P. Choo-Smith, H.G.M. Edwards, H.P. Endtz, J.M. Kros, F. Heule, H. Barr, J.S. Robinson, H.A. Bruining, and G.J. Puppels, Biopolymers 67(1), 1â9 (2002).
- Z. Movasaghi, S. Rehman, and I.U. Rehman, Appl. Spectrosc. Rev.42(5), 493â541 (2007).
- D.I. Ellis, D.P. Cowcher, L. Ashton, S. O’Hagan, and R. Goodacre, Analyst138(14), 3871â3884 (2013).
- I.R. Lewis and H.G.M. Edwards, Handbook of Raman Spectroscopy: From the Research Laboratory to the Process Line (CRC Press, New York, New York, 2001).
- Emerging Raman Applications and Techniques in Biomedical and Pharmaceutical Fields, part of Biological and Medical Physics, Biomedical Engineering series, M.D. Morris and P. Matousek, Eds. (Springer, Heidelburg, New York, 2010).
- A. Amin, P. Bourget, F. Ader, F. Vidal, C. Neuzillet, and A. Baillet-Guffroy, J. Raman Spectrosc.46(12), 1283â1290 (2015).
- C. Bazin, B. Cassard, E. Caudron, P. Prognon, and L. Havard, Int. J. Pharm. 494(1), 329â336 (2015).
- http://www.cdc.gov/niosh/topics/hazdrug/, accessed 19 April 2016.
- E.S. Baker and T.H. Connor, Am. J. Health. Syst. Pharm. 53(22), 2713â2723 (1996).
- T.H. Connor, P.J.M. Sessink, B.R. Harrison, J.R. Pretty, B.G. Peters, R.M. Alfaro, A. Bilos, G. Beckmann, M.R. Bing, L.M. Anderson, and R. DeChristoforo, Am. J. Health. Syst. Pharm.62(5), 475â484 (2005).
- J. Couch, J. Gibbins, and T.H. Connor, J. Occup. Environ. Hyg. 10(4), D45âD51 (2013).
- S. Mazurek and R.J. Szostak, Pharm. Biomed. Anal.40(5), 1235â1242 (2006).
- P. Bourget, A. Amin, A. Moriceau, B. Cassard,F. Vidal, and R. Clement, Pathol. Biol. 60(6), 369â379 (2012).
- A. Amin, P. Bourget, F. Vidal, and F. Ader, Int. J. Pharm. 474(1â2), 193â201 (2014).
- P. Bourget, A. Amin, F. Vidal, C. Merlette, P. Troude, and A. Baillet-Guffroy, Int. J. Pharm.470(1â2), 70â76 (2014).
- P. Bourget, A. Amin, F. Vidal, C. Merlette, and F. Lagarce, J. Pharm. Biomed. Anal.91, 176â184 (2014).
- F. Nardella, M. Beck, P. Collart-Dutilleul, G. Becker, C. Boulanger, L. Perello, A. Gairard-Dory, B. Gourieux, and G. Ubeaud-Séquier, Int. J. Pharm.499(1â2), 343â350 (2016).
- P. Bourget, A. Amin, F. Vidal, C. Merlette, P. Troude,and A. Baillet-Guffroy, Int. J. Pharm.470(1â2), 70â76 (2014).
- K. Buckley, C.G. Atkins, D. Chen, H.G. Schulze, D.V. Devine, M.W. Blades, and R.F.B. Turner, The Analyst141(5), 1678â1685 (2016).
- J. Weaver, Anesth. Prog. 58(3), 111â112 (2011).
- R.E. St John, Crit. Care Nurse23(4), 83â88 (2003).
- R. Garg and R.C. Gupta, Indian J. Anaesth. 57(5), 481â488 (2013).
- R.A. Van Wagenen, D.R. Westenskow, R.E. Benner, D.E. Gregonis, and D.L. Coleman, J. Clin. Monit.2(4), 215â222 (1986).
- D.R. Westenskow, K.W. Smith, M.D. D.L. Coleman, D.E. Gregonis, and R.A. Van Wagenen, Anesthesiology70(2), 350â355 (1989).
- D.E. Gregonis, R.A. Van Wagenen, D.; Coleman, and J.R. Mitchell, in Raman and Luminescence Spectroscopies in Technology II, F. Adar, and J.E. Griffiths, Eds. (Proceedings of SPIE, volume 1336, 1990), pp. 247â255.<
- J.R. Tobin, E.A. Spurrier, and R.C. Wetzel, Br. J. Anaesth. 69(5), 482â486 (1992).
- D. Lawson, S. Samanta, P.T. Magee, and D.E. Gregonis, J. Clin. Monit. 9(4), 241â251 (1993).
- https://www.woodlibrarymuseum.org/museum/item/754/rascal-ii, accessed 21 April 21, 2016.
- G.G. Lockwood, M.J. Landon, M.K. Chakrabarti, and J.G. Whitwam, Anaesthesia 49(1), 44â53 (1994).
- S. Sadhasivam and D. Lai, Bulletin of Anasthesia History, January 2004.
- A.J. Davey and A. Diba, Ward’s Anaesthetic Equipment (Elsevier Health Sciences, UK, 2012).
- S. Schlüter, F. Krischke, N. Popovska-Leipertz, T. Seeger, G. Breuer, C. Jeleazcov, J. Schüttler, and A. Leipertz, J. Raman Spectrosc. 46(8), 708â715 (2015).
- S. Schluter, F. Krischke, N. Popovska-Leipertz, T. Seeger, G. Breuer, C. Jeleazcov, J. Schüttler, and A. Leipertz, Laser Applications to Chemical, Security and Environmental Analysis 2014DOI: 10.1364/LACSEA.2014.LW4D.6 (OSA, Seattle, Washington, 2014), p LW4D.6.
- M. Pudlas, S. Koch, C. Bolwien, and H. Walles, Int. J. Artif. Organs 33(4), 228â237 (2010).
- Y. Takahashi, T. Shishido, K. Yamamoto, Y. Sawaji, J. Nishida, and G. Pezzotti, J.Raman Spectrosc.v46i11, 1166â1172 (2015).
- J.-D. P. McElderry, M.R. Kole,and M.D. Morris, J. Biomed. Opt.16(7), 071407â071407-4 (2011).
- R. Tandon and A.S. Herford, “Bone Graft Complications: What Can We Do to Prevent Them?” presented at SPIE Photonics West, San Francisco, California, 2014.
- T. Yamamoto, K. Uchida, K. Naruse, M. Suto, K. Urabe, K.Uchiyama, K. Suto, M. Moriya, M. Itoman, and M. Takaso, Cell Tissue Bank. 13(3), 409â414 (2011).
Karen A. Esmonde-White is with Kaiser Optical Systems, Inc., in Ann Arbor, Michigan and the University of Michigan Medical School, Department of Internal Medicine-Rheumatology in Ann Arbor. Direct correspondence to:
Articles in this issue
over 9 years ago
Evaluation of Eye Shadow Compounds Using Raman Microspectroscopyover 9 years ago
Using SERS to Study How Cells Respond to Pharmaceuticalsover 9 years ago
Tech Tip: Choosing Raman Excitation WavelengthsNewsletter
Get essential updates on the latest spectroscopy technologies, regulatory standards, and best practices—subscribe today to Spectroscopy.